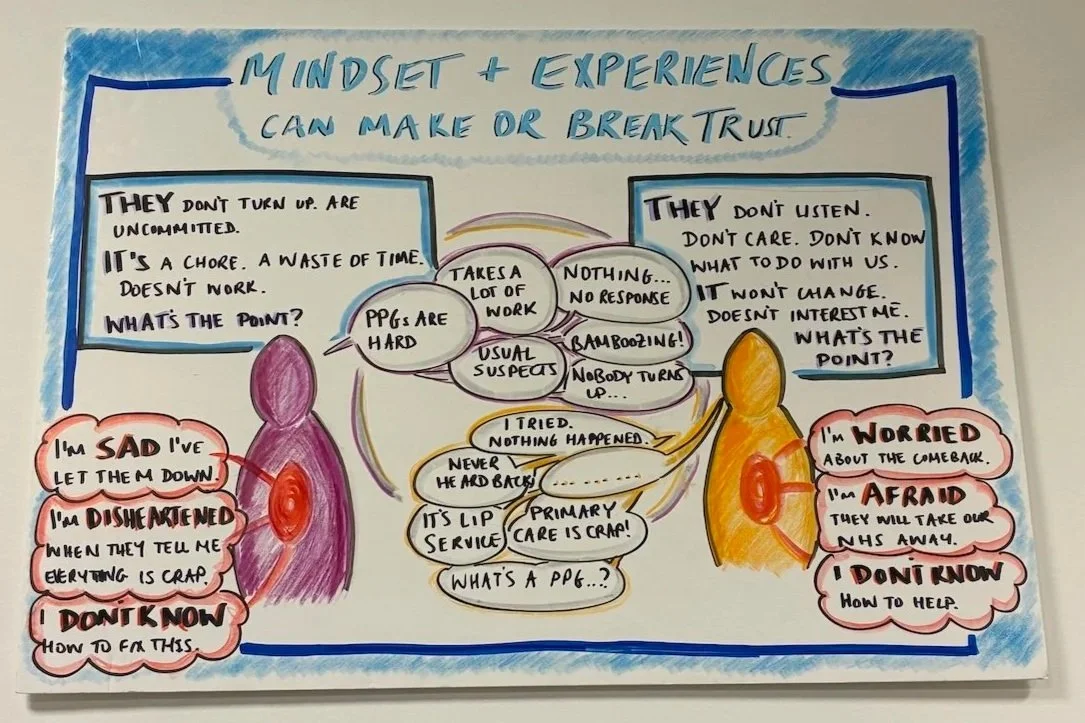
Mindset and experiences can make or break trust.
During our Open Studios in December, we pinned up a mix of boards and drawings from past projects. This one stayed up, and I now find myself looking at it while waiting for the coffee machine to run through.
It comes from a project work in 2018-19, working with Patient Participation Groups (PPGs) in East London. The board is a bit chaotic and scrappy. I’m an enthusiastic drawer, though not an especially polished one. I’ve kept it exactly as it is.
At the time, I was presenting to a CCG board (Clinical Commissioning Group, before the current ICBs [Integrated Care Boards]). It was a two-hour board meeting. I had 10 mins, which I was told would likely get squeezed with overrunning discussions. The meeting’s pre-reading pack was over 200 pages.
When my slot came, I stood up and held up my slightly scrappy drawing.
I used it describe this emerging narrative of “us” and “them” that was running through the work. We had been asked to work with 40 GP practices to improve their working relationships with their PPGs.
For many practices, it felt like a stalemate.
Patients would say: “they don’t listen to us”.
Staff would say: “we ask for feedback all the time. They never show up. These engagement sessions are a chore. It’s a waste of time. What’s the point?”
Patients would say: “They don’t know what to do with us. Nothing changes. Why would I come to a place where sick people go, just to help people do their jobs better?”
Staff would hear: “Primary care is crap! I can never get an appointment. It’s all lip service!”
But the quieter moments, after the waves of anger and frustration had passed, something else surfaced.
Among staff, I often heard sadness:
I’m sad I’ve let people down. This isn’t the service we want to provide.
It’s hard to hear that everything feels broken.
I don’t how to fix to this.
Among patients and community members, I heard fear and grief:
I’m worried about the comeback of speaking up. What if my care, or my children’s care, is affected?
I’m afraid they will take our NHS away.
I don’t know how to help them.
My intention in that CCG conversation was share insights to explore how co-production might work in practice. How could we get unstuck?
It was through projects like this that I learned the value of showing up with unconditional positive regard. But that, I mean holding care and respect for people on both ‘sides’ of the relationship: those who service the public, and those who rely on those services.
Again and again, this has felt like the strongest place to begin partnership working. And the place to return to when the misunderstandings, pressure and the realities of complex systems inevitably resurface emerges.
Thinking Out Loud is where I share short pieces of thinking from the middle of the work. Ideas, questions and lived experiences, shared while they’re still forming. (Tiny Experiments Pact: Day 9/100).